Drug overdoses killed 20 Manitobans aged 50 and over in April, as the number of fatalities returned to a near-record high with a warning over an emerging class of extremely potent synthetic opioids.
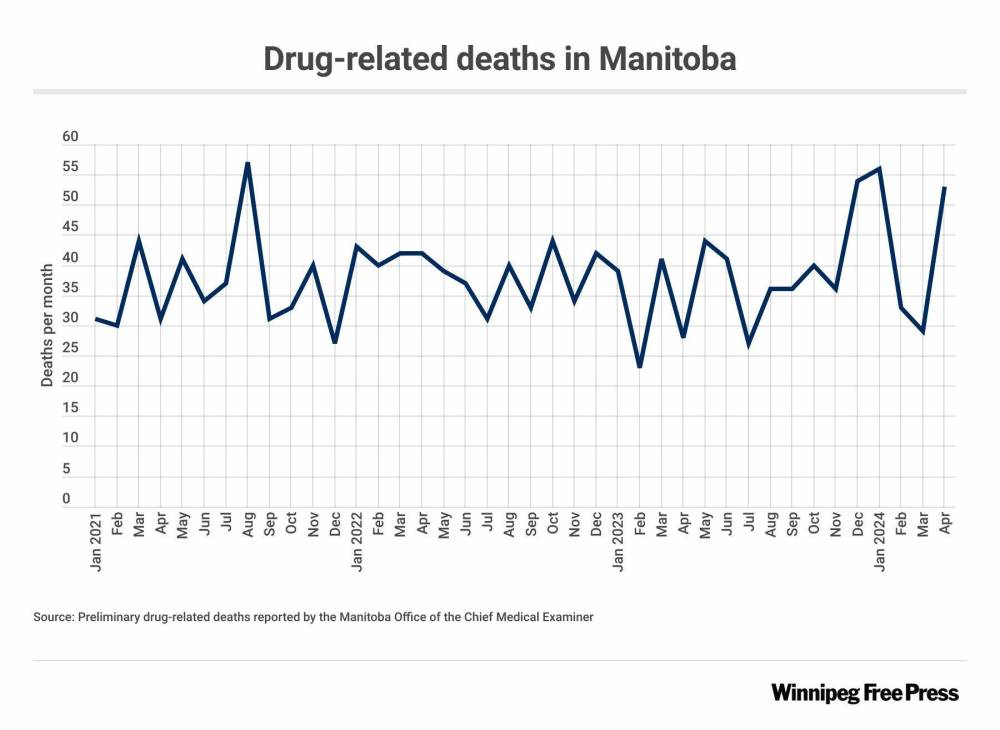
Manitoba recorded 53 suspected drug-related deaths that month, up from 29 in March and 33 in February, according to preliminary figures Wednesday from the Office of the Chief Medical Examiner.
“The first thing that comes to mind is sheer sadness,” said Levi Foy, executive director of Sunshine House, which operates Winnipeg’s lone mobile overdose prevention site. “These are human beings with connections, relationships and people who love them.”

(Liz O. Baylen/Los Angeles Times/TNS)
Manitoba recorded 53 suspected drug-related deaths in April, up from 29 in March and 33 in February, according to preliminary figures Wednesday from the Office of the Chief Medical Examiner.
“It saddens me, because these deaths are preventable,” said Arlene Last-Kolb, the Manitoba director of Moms Stop the Harm, a group of parents who’ve lost children to drug poisonings. “There is a rippling effect on our whole (province).”
January’s preliminary total of 56 deaths was the highest monthly figure since 57 were reported in August 2021.
Events are being held this week to mark International Overdose Awareness Day, which is officially Saturday, and remember people such as Last-Kolb’s 24-year-old son, Jessie, who died from a fentanyl overdose in 2014.
Addictions Minister Bernadette Smith is hosting a gathering at the legislature Friday.
“The increase in substance-related deaths in Manitoba is both staggering and heartbreaking,” she said in a statement. “These are not just numbers. They are our loved ones, neighbours, friends, partners, parents, and children. While we carry the weight of this grief together, it also compels us to seek and create solutions.”
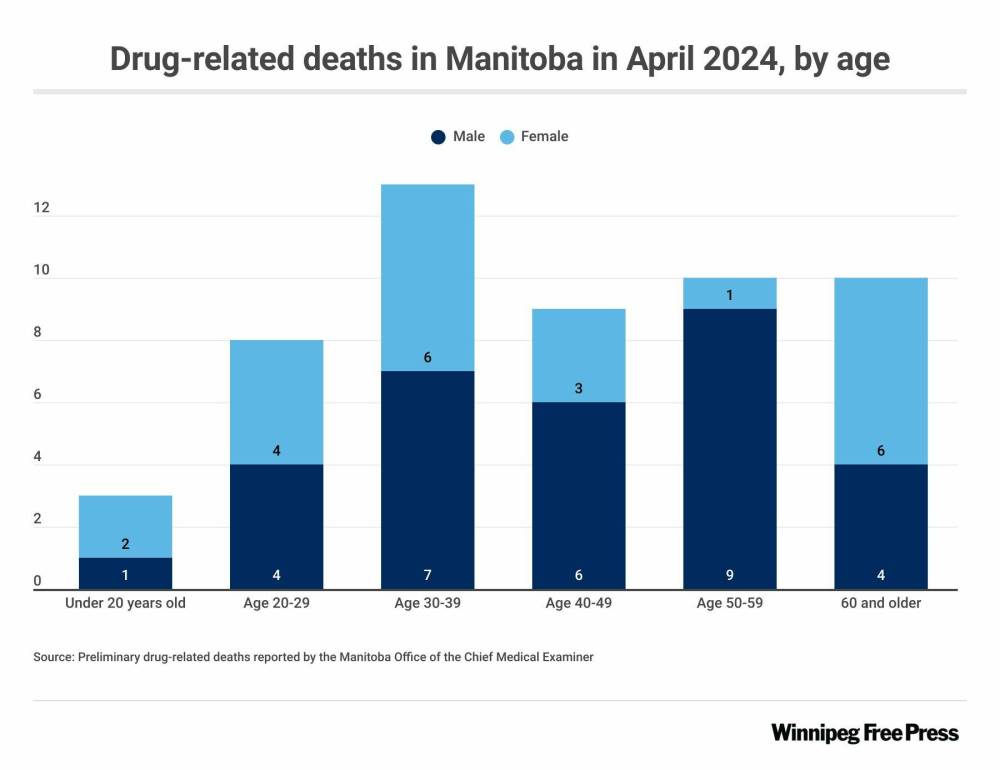
April brought an uptick in deaths in the chief medical examiner’s two oldest age categories. Ten people (nine men and one woman) were aged 50-59, and 10 (four men and six women) were 60 or over.
Three people were in the 0-19 age range, eight were in their 20s, 13 were 30-39 and nine were in their 40s.
Overall, 31 of those who died were male and 22 were female.
The chief medical examiner reported 32 deaths involving fentanyl, the synthetic opioid most associated with the toxic drug crisis.
Protonitazene — from the nitazene class of manufactured opioids — was detected in one case.
“Unfortunately, my expectation is that we will be seeing more of this class of drugs as time passes,” chief medical examiner director Kathryn Braun wrote in an email. “Manitoba tends to lag a couple of years behind B.C. in terms of what drugs we encounter; there is no reason to believe that this won’t also occur with the nitazenes.”
Braun said nitazenes were first developed in the 1950s, but never used in a clinical setting due to their extreme potency and high risk of respiratory and central nervous system depression.
“They began appearing in illicit drug preparations at least five years ago, primarily in the U.S., where they have become major problems in some jurisdictions,” she wrote. “There have been a fair number of drug-related deaths involving nitazenes in Ontario and B.C. in the last couple of years; Manitoba has only encountered these substances a handful of times overall.”
Some nitazenes are hundreds of times more potent than heroin or considerably more potent than fentanyl, said Braun.
“As such, they are extremely dangerous, especially to naïve opioid users,” she wrote. “My understanding is that naloxone would be effective to some degree, but would be required in vastly greater doses than in the case of heroin toxicity.”
Protonitazene — a controlled substance — was first detected in Canada in a sample seized by police in Quebec City in 2020, according to Health Canada.
Toronto’s Drug Checking Service said it identified protonitazene in that city’s unregulated opioid supply for the first time in March. The opioid was mixed into two powders that were expected to be but did not contain oxycodone.
“There’s always going to be something new coming out,” said Last-Kolb, who advocates for a safer-supply model, which provides users with drugs that have been tested, as an alternative to the toxic, illegal street supply. “Safe supply would not be offering these types of drugs.”
The province recently bought two new drug-testing machines to be operated by front-line street outreach workers.
Manitoba’s first supervised consumption site is expected to open in downtown Winnipeg in 2025. The Indigenous-led facility will provide primary medical care and support for addictions treatment and mental health counselling.
Premier Wab Kinew has also directed Smith to expand detox beds and addiction treatment options.
Foy said more work can be done to address root causes of drug-related deaths and better support people who are in various stages of addiction.
There is a need for more community-led programs, treatment or withdrawal management options, and housing and income supports, he said.
chris.kitching@freepress.mb.ca

Chris Kitching
Reporter
Chris Kitching is a general assignment reporter at the Free Press. He began his newspaper career in 2001, with stops in Winnipeg, Toronto and London, England, along the way. After returning to Winnipeg, he joined the Free Press in 2021, and now covers a little bit of everything for the newspaper. Read more about Chris.
Every piece of reporting Chris produces is reviewed by an editing team before it is posted online or published in print — part of the Free Press‘s tradition, since 1872, of producing reliable independent journalism. Read more about Free Press’s history and mandate, and learn how our newsroom operates.
Our newsroom depends on a growing audience of readers to power our journalism. If you are not a paid reader, please consider becoming a subscriber.
Our newsroom depends on its audience of readers to power our journalism. Thank you for your support.