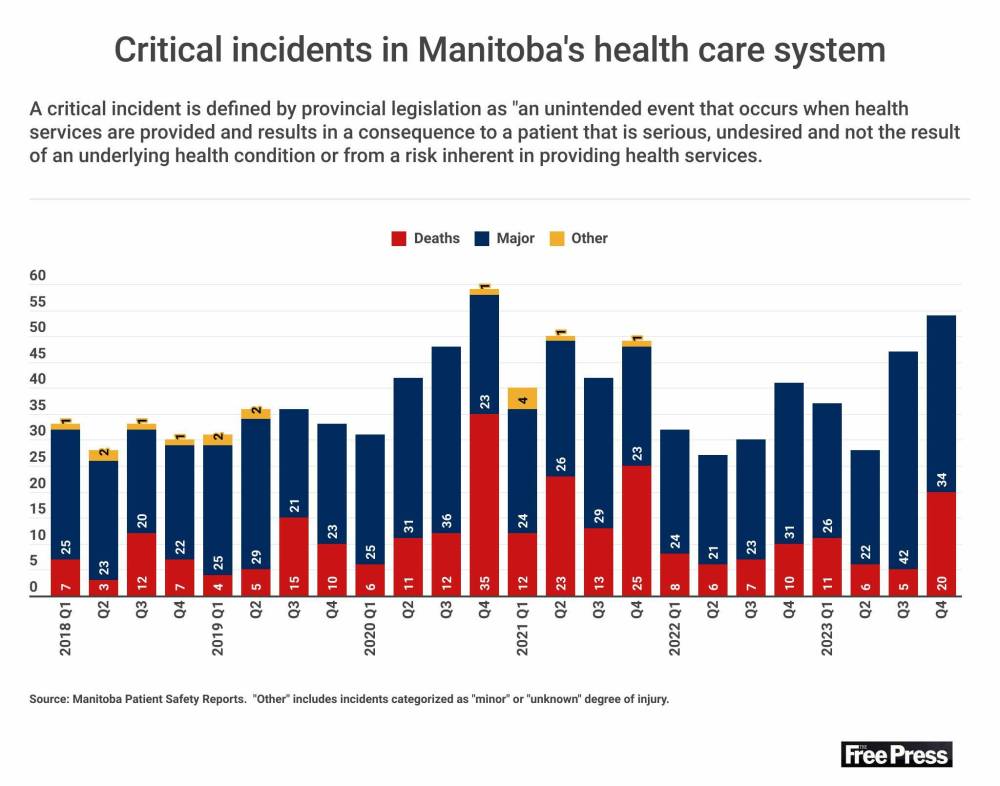
The number of critical incidents in Manitoba’s health-care system in late 2023 soared to the highest level since early in the COVID-19 pandemic, with delays or missed opportunities cited in many cases.
Manitoba Health’s latest quarterly report, published online this week, listed 54 incidents, including 20 deaths, between Oct. 1 and Dec. 31.
It was the highest quarterly total since the same three-month period in 2020, when 59 incidents (35 deaths) resulted in “serious and unintended” harm to people using health-care services.
Manitoba Nurses Union president Darlene Jackson pointed to an increase in incidents involving delays or missed opportunities.
“This is about delays in care or moving to a higher level of care because deterioration was not recognized,” she said Friday. “I’m seeing a lot more of that here in this report.”
The final quarterly report of 2023 showed a calendar year-over-year rise in incidents and deaths.
The province listed 166 critical incidents, including 42 deaths, last year, up from 130 incidents (31 deaths) in 2022, based on an analysis of public reports.
Totals were higher in 2021 (181 incidents, 73 deaths) and 2020 (180 incidents, 64 deaths).
Critical incidents related to COVID-19 outbreaks in hospitals or personal-care homes were reported as groups in 2021 and 2022.
Critical Incidents Reported to Manitoba Health: October 1, 2023 – December 31, 2023
Jackson and Jason Linklater, president of the Manitoba Association of Health Care Professionals, attributed the increase in incidents to chronic staff shortages and high patient ratios and workloads.
“We continue to see the upward trend and, frankly, it’s not surprising, with the huge net loss of staff that occurred within those years,” said Linklater.
He said the staffing crisis is creating dangerous situations for patients and health-care employees, with delays or preventable incidents more likely to occur when staffing numbers are lower.
“It’s a really difficult thing to mitigate risk when you don’t have adequate numbers of professionals providing care,” said Linklater, whose union represents about 7,000 workers, including rural paramedics and lab and diagnostic technologists.
Jackson said nurses are stretched thin and unable to monitor individual patients as frequently as needed.
“You need to be monitoring frequently to pick up on this,” said Jackson.
She said her heart goes out to patients and families affected by critical incidents, and nurses who leave work feeling defeated or they weren’t able to do more because there wasn’t enough staff.
“It causes so much moral distress,” said Jackson.

RUTH BONNEVILLE / FREE PRESS FILES
“This is about delays in care or moving to a higher level of care because deterioration was not recognized,” said Darlene Jackson, president, Manitoba Nurses Union.
Of the 20 deaths, one patient suffered delays in recognition and treatment for an acute medical condition, while another experienced a delay in diagnosis of a serious medical condition.
The report said two people died following gaps in monitoring. One death involved a delay in response to a deteriorating patient.
A patient who sought help for an acute medical condition died after a delay in transfer to a higher level of care. A client died after a fall resulted in fractures.
Non-fatal incidents included a person who suffered severe harm after being unable to access medical care, a patient whose condition worsened due to gaps in treatment, a skin wound that resulted in amputation, and a client who suffered a fracture when struck by a “co-client.”
Jackson said staff retention must be the top priority, because the impacts of high workloads are driving nurses out of the public system.
“We’re in a critical shortage, and we have a finite number of nurses. We need to keep those nurses that are here at whatever cost,” she said.
Training more nurses will help, but it’s a “four-year plan,” based on the length of time it takes to train nurses, said Jackson.
Linklater agreed retention is key.
“We simply cannot afford to lose more, while working on long-term solutions,” he said.
Linklater said there has been a net gain of 52 allied workers in 2024 as of July, compared with net losses of 17 in 2023 and 100 in 2022.
Before then, the system was short 1,000 allied professionals, he said.
Linklater said a major contributor to the exodus of staff was a five-year period in which MAHCP members worked without a contract under the former Progressive Conservative government.
Staff are again without a contract as of April 1.
The latest critical incident report covers the transition between PC and NDP governments after last October’s election.
Provincial legislation defines a critical incident as an unintended event “that occurs when health services are provided to an individual and results in a consequence to him or her that is serious and undesired.”
This can include a death, injury or disability that does not result from the person’s underlying health condition “or from a risk inherent in providing the health services.”
Critical incident reports provide a limited description for each death or major event. Information that could identify patients or staff — names, specific medical conditions, dates and locations — is withheld.
The public posting of reports is intentionally delayed by a minimum of six months to allow time for a review of each incident and final disclosure.
Reports do not disclose any measures taken to prevent similar deaths or injuries. The findings of investigations, and any recommendations, are shared internally, according to the province.
“One critical incident is too many. And when reviewing these it’s obvious the strain on the system has been building for years.”–Health Minister Uzoma Asagwara
Recommendations, or patient-safety learning advisories, have not been published online since 2019.
A new standard template for PSLAs is being implemented across all Manitoba health authorities, a provincial spokesperson said.
Shared Health is developing a new webpage where PSLAs will be shared with the public, the spokesperson said.
The page is expected to launch in time for Canadian Patient Safety Week, which begins Oct. 28.
“One critical incident is too many. And when reviewing these it’s obvious the strain on the system has been building for years,” Health Minister Uzoma Asagwara told the Free Press in a statement.
“But these reports are important, to help us learn what we can do better. That’s why we moved to capturing the data faster and sharing with the public sooner.”
Linklater said details about preventative actions should be shared with Manitobans.
“It’s important for the public to be able to read reports and decipher why and where problems occur,” he said. “When you look at the information provided, you can’t decipher that.”
chris.kitching@freepress.mb.ca

Chris Kitching
Reporter
Chris Kitching is a general assignment reporter at the Free Press. He began his newspaper career in 2001, with stops in Winnipeg, Toronto and London, England, along the way. After returning to Winnipeg, he joined the Free Press in 2021, and now covers a little bit of everything for the newspaper. Read more about Chris.
Every piece of reporting Chris produces is reviewed by an editing team before it is posted online or published in print — part of the Free Press‘s tradition, since 1872, of producing reliable independent journalism. Read more about Free Press’s history and mandate, and learn how our newsroom operates.
Our newsroom depends on a growing audience of readers to power our journalism. If you are not a paid reader, please consider becoming a subscriber.
Our newsroom depends on its audience of readers to power our journalism. Thank you for your support.